The Robo-Medic: Can AI Solve the Organ Shortage Crisis?
"Life finds a way." This iconic line from Jurassic Park echoes a profound truth: nature is resilient, but can humanity accelerate this resilience with technology? Imagine a world where waiting lists for organ transplants are relics of the past—a world where artificial intelligence (AI) and 3D bioprinting merge to create custom-grown organs tailored to each patient. This is not the stuff of science fiction; it is the frontier of modern medicine.
Organ shortages are a global crisis. According to the World Health Organization, only 10% of the global need for organ transplants is met annually, leading to over 8 deaths every hour. Enter the Robo-Medic—a concept where AI-driven systems revolutionize organ transplantation by growing organs on demand. This article explores how AI is reshaping 3D bioprinting, the challenges and breakthroughs in this field, and whether these technologies can finally solve the organ shortage crisis.
Luminaries like Ray Kurzweil, the futurist and Google’s Director of Engineering, have long predicted the convergence of AI and biotechnology. Similarly, Jennifer Doudna, the Nobel Prize-winning biochemist behind CRISPR, has highlighted the potential of AI in advancing genetic engineering. Even Elon Musk, the tech mogul behind Neuralink, has hinted at the transformative power of AI in healthcare. Their collective vision is clear: the future of medicine lies at the intersection of biology and technology.
1. The Global Organ Shortage Crisis: A Looming Epidemic
1.1 The Scale of the Problem
Every year, over 100,000 people in the United States alone are added to the organ transplant waiting list. Globally, the numbers are staggering. The World Health Organization estimates that less than 10% of the global demand for organs is met, leaving millions to suffer or die while waiting. In countries like India and China, the gap is even wider due to cultural and logistical barriers to organ donation.
Consider this: every hour, 8 people die waiting for an organ transplant. That’s like losing an entire soccer team every 90 minutes. The numbers are grim, but they highlight the urgency of finding a solution. Traditional organ donation systems, while noble, are simply not keeping up with the demand.
1.2 The Limitations of Traditional Solutions
Organ donation is a beautiful act of generosity, but it’s not without its flaws. For starters, there’s the issue of compatibility. Even if a donor is willing, their organs might not match the recipient’s blood type or tissue type. Then there’s the logistical nightmare of transporting organs quickly enough to ensure they remain viable. A heart, for example, can only survive outside the body for about 4-6 hours.
Living donors are another option, but they come with their own set of challenges. Not everyone is physically or emotionally prepared to donate a kidney or a portion of their liver. And let’s not forget the ethical dilemmas—should a healthy person risk their life to save another? These questions have no easy answers, which is why we need to look beyond traditional solutions.
1.3 The Urgent Need for Innovation
When the status quo is failing, innovation becomes a necessity. The organ shortage crisis isn’t just a medical problem—it’s a humanitarian one. Every life lost is a tragedy, and every day we delay finding a solution is a day too many. This is where technology steps in. By leveraging advancements in AI and 3D bioprinting, we can create a future where organs are grown on demand, tailored to each patient’s unique needs.
Think of it like this: if nature can grow a heart in nine months, why can’t we grow one in nine weeks—or even nine days? With the right tools and a bit of ingenuity, the impossible becomes possible. The Robo-Medic isn’t just a dream; it’s a call to action. The question is, are we ready to answer it?
2. The Rise of 3D Bioprinting: A Game-Changer in Medicine
2.1 What is 3D Bioprinting?
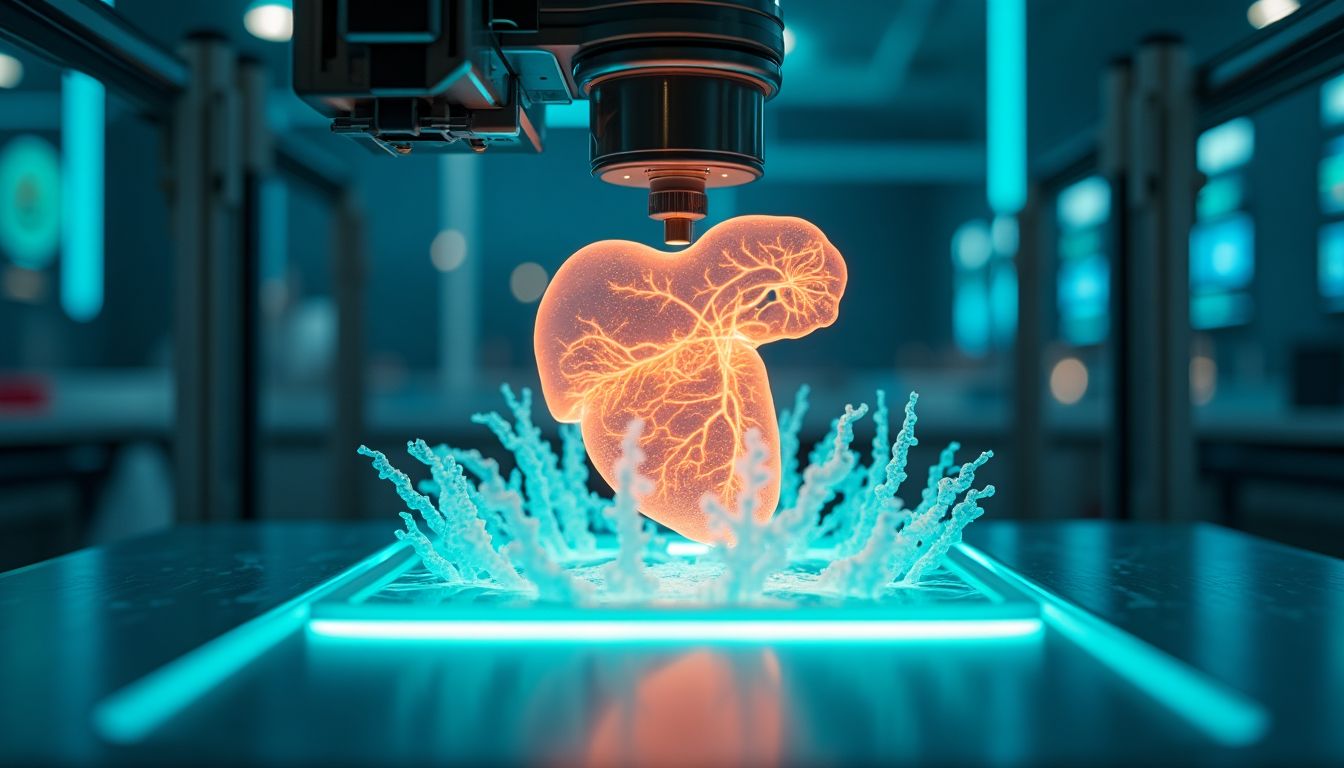
Imagine a printer, but instead of spitting out paper, it creates living tissues and organs. That’s 3D bioprinting in a nutshell. Unlike your average office printer, bioprinters use bioinks—materials made of living cells—to build structures layer by layer. Think of it as building a LEGO set, but with cells instead of plastic bricks. The result? Custom-made tissues and organs tailored to individual patients. It’s like science fiction, but it’s happening right now in labs around the world.
2.2 The Evolution of Bioprinting Technology
Bioprinting didn’t just appear overnight. It’s the result of decades of research and innovation. The first bioprinter was developed in the early 2000s, and since then, the technology has evolved faster than a teenager’s TikTok feed. Key players like Organovo and CELLINK have been at the forefront, pushing the boundaries of what’s possible. Institutions like the Harvard Wyss Institute and Stanford Bio-X are also making waves with groundbreaking research. It’s a race to the future, and the finish line is a world where organ shortages are a thing of the past.
2.3 Current Applications and Success Stories
So, what can bioprinting do right now? A lot, actually. Scientists have successfully bioprinted skin, cartilage, and even simple organs like bladders. These creations aren’t just lab curiosities—they’re being used in real-world applications. For example, bioprinted skin is helping burn victims recover faster, and bioprinted cartilage is being tested for joint repairs. But the real excitement lies in the future. Researchers are working on bioprinting more complex organs like kidneys and livers. It’s like upgrading from a flip phone to a smartphone—except the smartphone is a fully functional organ.
3. AI’s Role in 3D Bioprinting: The Brain Behind the Machine
3.1 How AI Enhances Bioprinting
If bioprinting is the body, AI is the brain. Artificial intelligence is supercharging bioprinting by optimizing designs and speeding up the development process. Imagine trying to solve a Rubik’s Cube blindfolded—it’s tough, right? Now imagine having a supercomputer that can solve it in seconds. That’s what AI does for bioprinting. It analyzes vast amounts of data to create the perfect organ design, ensuring that every cell is in the right place. It’s like having a GPS for organ creation.
3.2 Machine Learning and Organ Development
Machine learning, a subset of AI, is particularly powerful in predicting how cells will behave. By training AI models on data from thousands of organ samples, scientists can predict how a bioprinted organ will function before it’s even made. This is crucial for personalizing organs for individual patients. Think of it as tailoring a suit—except the suit is a kidney, and the tailor is a computer. It’s a game-changer for ensuring compatibility and reducing the risk of rejection.
3.3 Challenges in AI-Driven Bioprinting
Of course, it’s not all smooth sailing. There are ethical concerns, like who gets access to these life-saving technologies and how they’re regulated. There are also technical challenges, like ensuring that bioprinted organs have functional blood vessels. And let’s not forget the regulatory hurdles—getting approval for new medical technologies is like running a marathon with hurdles. But despite these challenges, the potential benefits are too great to ignore. It’s like climbing a mountain—tough, but the view from the top is worth it.
4. The Science of Growing Organs: From Cells to Complex Structures
4.1 Understanding Organogenesis
Organogenesis is the process by which organs develop naturally in the human body. It’s a complex dance of cells, signals, and time that results in fully functional organs. To understand how we might replicate this process in the lab, scientists study how cells communicate, differentiate, and organize themselves during development. For example, during the formation of the heart, cells known as cardiomyocytes come together to form the muscle tissue that pumps blood throughout the body. Researchers at institutions like the Harvard Wyss Institute are working to mimic these natural processes using AI and bioprinting.
4.2 The Role of Stem Cells
Stem cells are the building blocks of organogenesis. These versatile cells have the ability to develop into any type of cell in the body, making them essential for bioprinting organs. There are two main types of stem cells used in bioprinting:
- Embryonic Stem Cells (ESCs): Derived from early-stage embryos, these cells are highly versatile but come with ethical concerns.
- Induced Pluripotent Stem Cells (iPSCs): Created by reprogramming adult cells, iPSCs avoid ethical issues and can be tailored to individual patients.
Companies like STEMCELL Technologies are at the forefront of advancing stem cell research, but challenges remain in ensuring these cells can fully mature into functional tissues.
4.3 Building Vascular Networks
One of the biggest hurdles in bioprinting complex organs is creating a functional vascular system—the network of blood vessels that deliver oxygen and nutrients. Without this, bioprinted organs cannot survive or function properly. Recent breakthroughs, like those from researchers at the Stanford Bio-X program, have shown promising results in printing vascular networks using advanced materials and techniques. These innovations are bringing us closer to creating fully functional, life-saving organs.
5. The Ethical, Legal, and Social Implications of AI-Driven Organ Creation
5.1 Ethical Dilemmas
The idea of creating organs in a lab raises significant ethical questions. For example, who owns the rights to a bioprinted organ? Could this technology be misused for unethical purposes, like creating organs for profit or enhancing human abilities beyond natural limits? Organizations like the World Health Organization (WHO) are calling for global ethical guidelines to ensure this technology is used responsibly. As we move forward, it’s crucial to balance innovation with moral considerations.
5.2 Legal and Regulatory Considerations
Currently, there are no international standards governing AI-driven bioprinting. This lack of regulation could lead to inconsistencies in safety and quality. Governments and institutions must work together to establish clear laws, like those being proposed by the U.S. Food and Drug Administration (FDA), to ensure bioprinted organs meet rigorous standards. Without these safeguards, the technology could face public backlash or even be banned.
5.3 Public Perception and Acceptance
How people view AI-driven organ creation will play a critical role in its success. While some may see it as a miraculous solution to the organ shortage crisis, others might fear the unknown or distrust technology in medicine. Surveys conducted by institutions like the Pew Research Center show that public acceptance of AI in healthcare is growing, but there’s still work to be done. Building trust through transparency, education, and real-world success stories will be key to widespread adoption.
6. AI Solutions: The Blueprint for a New Era of Organ Creation
6.1 Data Integration and Analysis
The foundation of AI-driven organ creation lies in the ability to harness vast datasets. By integrating data from NCBI and other biomedical repositories, AI can analyze organ biology at an unprecedented scale. This allows for the optimization of bioprinting protocols, ensuring that each organ is tailored to the patient’s unique needs.
6.2 Design Optimization
Using advanced algorithms, AI can create intricate, patient-specific organ designs. By simulating the natural development process, AI ensures that each organ is structurally sound and functional. This approach minimizes the risk of rejection and maximizes the chances of a successful transplant.
6.3 Automating Bioprinting Processes
AI can streamline the bioprinting process by automating key steps. From material selection to layer-by-layer fabrication, AI-driven robotics can ensure precision and efficiency. This not only reduces the time required but also minimizes human error, making the process more reliable.
6.4 Predictive Modeling
One of the most powerful applications of AI in bioprinting is predictive modeling. By simulating organ behavior, AI can ensure functionality and compatibility before the organ is even printed. This predictive capability is crucial for reducing the risk of post-transplant complications.
6.5 Accelerating Research
AI can identify new materials and techniques for organ development by analyzing existing research. By expediting the discovery process, AI can help bring new bioprinting technologies to market faster, ensuring that patients benefit from the latest advancements.
6.6 Action Schedule/Roadmap (Day 1 to Year 2)
Day 1: Assemble a multidisciplinary team of AI experts, bioprinting specialists, and medical researchers. Key collaborators include Harvard Wyss Institute, Stanford Bio-X, MIT Media Lab, and companies like Organovo and CELLINK.
Day 2: Conduct a comprehensive review of existing bioprinting technologies and AI applications in medicine. This will serve as the foundation for future developments.
Week 1: Develop a data repository for organ biology and bioprinting research. This repository will be the backbone of all data-driven AI models.
Week 2: Begin training AI models on organ development and bioprinting processes. This will involve feeding the AI vast amounts of data to ensure it can make accurate predictions.
Month 1: Design and prototype a bioprinter enhanced with AI capabilities. This will involve integrating AI algorithms into the bioprinting process to automate key steps.
Month 2: Test the AI-driven bioprinter on simple tissues like skin and cartilage. This will provide valuable insights into the technology’s capabilities and limitations.
Year 1: Conduct clinical trials for AI-designed tissues and simple organs. These trials will be crucial for gaining regulatory approval and ensuring patient safety.
Year 1.5: Expand trials to include more complex organs like kidneys or livers. This will be a significant milestone, demonstrating the technology’s potential to address the organ shortage crisis.
Year 2: Evaluate the success of AI-driven organ creation and refine technologies for widespread adoption. This will involve continuous improvement and optimization to ensure long-term success.
A Future Without Waiting Lists: The Promise of AI-Driven Organ Creation
The fusion of AI and 3D bioprinting holds the potential to transform healthcare, eliminating the organ shortage crisis and saving countless lives. Imagine a world where waiting lists for organ transplants are relics of the past—a world where custom-grown organs are the norm rather than the exception. This is not a distant dream but a future that is rapidly taking shape thanks to the advancements in AI and bioprinting technologies.
While challenges remain, such as ethical concerns and regulatory hurdles, the rapid pace of innovation suggests that these barriers can be overcome. The collaboration between leading institutions like Harvard Wyss Institute, Stanford Bio-X, and MIT Media Lab is driving this revolution, making the concept of the Robo-Medic a reality.
As we look to the future, it’s clear that AI-driven organ creation will play a pivotal role in addressing one of the most pressing issues in modern medicine. By leveraging AI’s predictive capabilities, automating the bioprinting process, and continuously improving through data-driven insights, we can ensure that every patient in need of an organ transplant has access to life-saving solutions.
The Robo-Medic is not just a concept—it is the next frontier of medicine. It represents a future where technology and humanity converge to create a healthier, more equitable world. So, are we ready to embrace this new era of innovation? Are we prepared to redefine what’s possible in medicine? The answers to these questions will shape the future of healthcare and the lives of millions around the globe.
What are your thoughts on the potential of AI-driven organ creation? Share your insights in the comments below, and don’t forget to subscribe to our newsletter to become a permanent resident of iNthacity: the "Shining City on the Web". Let’s continue this conversation and explore the limitless possibilities of technology together.
FAQ
Q1: How does 3D bioprinting work?
3D bioprinting is like using a high-tech printer, but instead of ink, it uses something called "bioinks." These bioinks are made of living cells. The printer layers these cells to create tissues or even whole organs. Think of it like building a cake layer by layer, but instead of frosting, you’re using living cells. The process is guided by AI algorithms that ensure everything is placed just right. Companies like Organovo and CELLINK are leading the way in this technology.
Q2: Are bioprinted organs safe for transplantation?
Right now, bioprinted organs are still in the testing phase. Early results are promising, but scientists need to make sure they’re completely safe before they can be used in people. This means a lot of clinical trials and checks to ensure the organs work properly and don’t cause any harm. It’s like testing a new car model to make sure it’s road-ready before selling it to the public.
Q3: How long before AI-driven organ creation becomes mainstream?
Experts think it could take anywhere from 5 to 10 years before AI-driven organ creation becomes widely available. This depends on how fast technology advances and how quickly regulatory bodies approve these new methods. It’s like waiting for a new smartphone to go from prototype to store shelves—there’s a lot of testing and refining involved.
Q4: What are the biggest challenges in AI-driven bioprinting?
There are a few big hurdles to overcome:
- Vascularization: Creating blood vessels that keep the organ alive and functioning.
- Ethical Concerns: Making sure AI is used responsibly in medicine.
- Technical Limits: Improving the precision and speed of bioprinting machines.
Institutions like the Harvard Wyss Institute and Stanford Bio-X are working hard to tackle these challenges.
Q5: Can AI create any type of organ?
Right now, AI and bioprinting can create simpler tissues like skin and cartilage. More complex organs like hearts or lungs are still in the experimental stage. It’s like learning to bake—you start with cookies before moving on to a multi-tiered wedding cake. Researchers at places like the MIT Media Lab are pushing the boundaries to make complex organs a reality.
Q6: How much will a bioprinted organ cost?
The cost is still unclear, but it’s expected to be high at first, just like any new technology. Over time, as the process becomes more efficient, prices should drop. Think of it like the first flat-screen TVs—they were super expensive, but now they’re affordable for most people. Companies like CELLINK are working to make bioprinting more cost-effective.
Q7: Will bioprinted organs be rejected by the body?
One of the biggest advantages of bioprinting is that organs can be made using a patient’s own cells. This significantly reduces the risk of rejection, which is a common problem with traditional transplants. It’s like giving your body a spare part that’s a perfect match, rather than one that might not fit quite right.
Q8: Who is leading the research in AI-driven bioprinting?
Several top institutions and companies are at the forefront of this research:
These groups are collaborating to push the boundaries of what’s possible in medicine.
Q9: What happens if AI makes a mistake in bioprinting?
AI systems are designed to be highly accurate, but they’re not perfect. If a mistake happens, it could mean the organ doesn’t work as intended. That’s why there are multiple checks and balances in place, including human oversight. It’s like having a co-pilot in a plane—AI does most of the work, but humans are there to step in if needed.
Q10: How can I stay updated on AI-driven bioprinting advancements?
You can follow leading research institutions and companies on their social media platforms or websites. For example:
You can also subscribe to our newsletter to get the latest updates on this groundbreaking technology.
Wait! There's more...check out our gripping short story that continues the journey: The Vermillion Heart
Disclaimer: This article may contain affiliate links. If you click on these links and make a purchase, we may receive a commission at no additional cost to you. Our recommendations and reviews are always independent and objective, aiming to provide you with the best information and resources.
Get Exclusive Stories, Photos, Art & Offers - Subscribe Today!

























Post Comment
You must be logged in to post a comment.